Asthma Bronchitis Breathing Beyond Limits
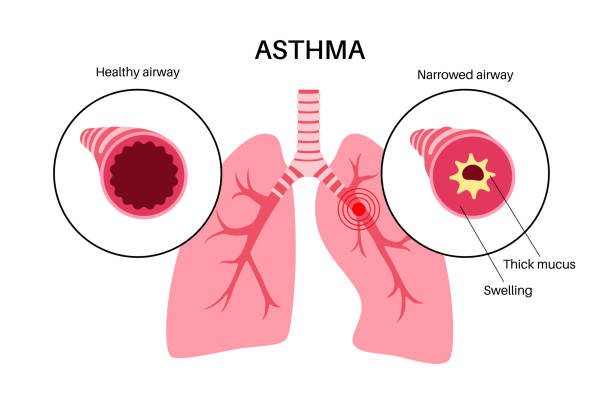
A common respiratory condition that poses a serious health risk, particularly to adults, is asthma bronchitis. The lower respiratory tract is affected by the disease, especially the bronchi, which are the primary airways that supply air to the lungs. When there is no sign of pneumonia, asthma bronchitis is characterized by bronchial inflammation. It usually affects those who have no underlying chronic obstructive lung disease (COPD). The signs of asthma bronchitis are the sudden onset of a chronic cough that is not accompanied by or with or without sputum production. Since it is a self-limiting illness, it usually follows a non-sensical process, that resolves spontaneously in one to three weeks. The root cause is inflammation in the respiratory tract of the lower part, which is usually triggered by viral infection.
Aetiology of Asthma Bronchitis

- Influenza, RSV, and human coronaviruses usually show their highest prevalence in winter. In the past, characteristic patterns of winter occurred because people stayed indoors more often and were in closer interpersonal contact, resulting in an environment that favours the rapid spread of these diseases.
- Rhinoviruses generally experience their highest frequency during the autumn and spring seasons, which coincide with changes in the weather patterns. Allergies during the season can cause these spikes through the possibility of facilitating transmission of the virus at the time.
- Enteroviruses in Asthma Bronchitis include various viruses that cause stomach and respiratory ailments to peak in the summer. This increase is correlated with an increase in outdoor activities, creating more chances to transmit viral infections.
The status of vaccination, especially for viruses such as influenza, may influence the causes of acute chronic bronchitis. A study carried out in France found that of more than 164 instances of asthma bronchitis among adult patients who had received an influenza vaccine, 37% of them were found to have a viral cause. The causes were identified as viral; two-thirds of the cases were linked to rhinovirus. The fact that, despite having been vaccination-free against influenza, some might still be susceptible to rhinovirus infections. These may manifest as symptoms of bronchitis. Exposure to irritating substances like fumes, air pollution dust, and pollutants in the environment can result in asthma, bronchitis, or aggravation of existing respiratory ailments. In addition, allergens may cause an allergic reaction within the airways that can result in inflammation, and the beginning of symptoms associated with bronchitis, especially when people are vulnerable to triggers like these.
Asthma Bronchitis Statistical Analysis
Physical and Historical

- At first, the cough might begin to be painful and dry. However, when acute bronchitis progresses, it may begin producing sputum. When bronchitis is severe, the cough can last for longer and can last for up to five days. About 50% of patients suffering from acute bronchitis experience an increase in sputum production. A prolonged or abrasive cough can result in chest wall or substernal muscle discomfort, which is usually self-limiting.
- Mild fever: A low-grade fever could be observed with both of these conditions, but it’s typically connected with respiratory infections of the upper part of the body. High-grade fevers during asthma and bronchitis are uncommon and should be investigated further.
- Aches and fatigue in the body General body discomfort is common with mild upper respiratory illnesses as well as acute respiratory bronchitis.
The distinction between the two situations becomes apparent when the condition progresses. When the symptoms are predominantly affecting your upper respiratory tract, and disappear within a couple of days, it’s more likely to be an upper respiratory illness. If the symptoms last over some time, say a week or more, and accompany lower respiratory tract issues, the signs are indicative of an acute case of lung inflammation. A physical exam of the lung’s auscultation can show wheezing. Sometimes the rhonchi detection could improve or be cleared by coughing. This suggests that breathing obstructions or airway secretions that cause the noise can be eliminated by a coughing effort. The possibility of pneumonia is a possible diagnosis when you notice the presence of rales or egophony. A mild tachycardia can be a sign of the symptoms, which could indicate an increase in temperature and dehydration as a result of the viral infection. It is crucial to remember that similar symptoms of tachycardia can be found when there are bacterial-related infections. The general evaluation of the other systems of the body is typically within the normal range. When it comes to managing asthma Bronchitis teams of healthcare professionals comprised of pharmacists, doctors, nurses as well as other healthcare professionals can be crucial in providing patient-centered healthcare, increasing outcomes, assuring patient safety, and maximizing the performance of the team. To achieve these objectives, the team must employ diverse strategies and skills to uphold ethical standards as well as accept shared responsibilities. promote open and transparent communication among professionals and effectively coordinate care. These are the key elements for increasing the effectiveness of the healthcare team in managing acute bronchitis. Every member of the team should have the knowledge and skills that are relevant to their job in the treatment of acute bronchitis. Doctors must be skilled in diagnosing and treating options, nurses must excel in monitoring and educating patients; and pharmacists must be knowledgeable about the management of medications as well as potential interactions with drugs. They have to continually comply with research-based suggestions and the maximum present-day strategies for diagnosing and treating acute respiratory bronchitis. Being up to date with present-day research and guidelines is crucial to imparting super hospital therapy. Defined roles and responsibilities in the group are crucial. Physicians determine and prescribe treatments, and nurses educate patients and follow up on their progress. Pharmacists make sure that patients are safe with the use of medications, and many other specialists contribute their expert expertise. For the affected person’s effects to be maximized, care coordination is essential. This includes scheduling follow-up visits, ensuring that remedy regimens are accompanied, and actively involving sufferers in health decision-making. When it involves teaching sufferers approximately preventative measures and the treatments for their medical conditions, nurses are important. Instilling information in patients will encourage active involvement in their healthcare and may result in a higher outcome. Physicians must review their regimens of medication to determine potential interactions as well as allergies to help reduce adverse reactions to drugs and enhance the safety of patients. Patients suffering from persistent illness should schedule follow-up appointments promptly for a review of progress and to consider alternatives if needed. This highlights the need for continuous care. An asthma bronchitis condition can result in the highest rate of mortality in patients who have underlying COPD as well as other pulmonary ailments. It is essential to realize that if symptoms last over 6 weeks, it is required to validate the validity of the initial diagnosis and to assess the possible possibility of the presence of other complications.



